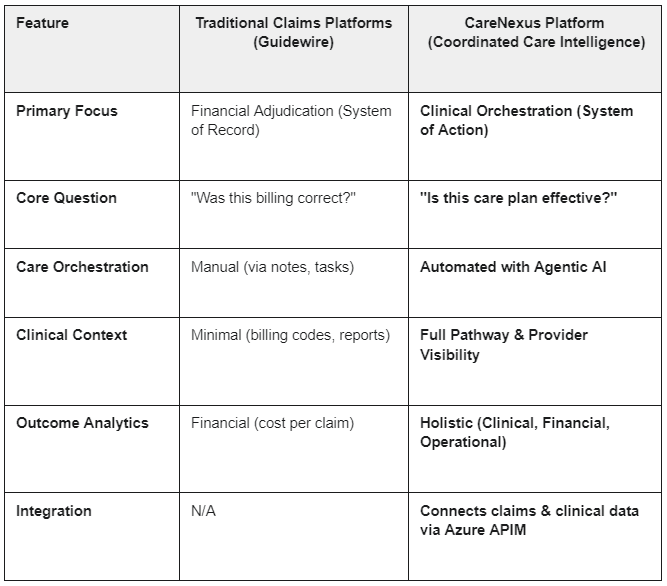
Claims management platforms like Guidewire have long been the backbone of insurance operations, ensuring financial accuracy and compliance. Yet, as healthcare costs rise and recovery timelines lengthen, these systems reveal a critical gap: they do not orchestrate care. They react after the fact, leaving payers blind to the clinical and operational drivers of cost.
The industry is responding. Organizations such as the Workplace Safety and Insurance Board (WSIB) are investing in care coordinators to manage worker journeys—a clear signal that proactive care orchestration is becoming strategic. But manual coordination is expensive, inconsistent, and difficult to scale.
This paper introduces Coordinated Care Intelligence as the next category of innovation. Powered by Agentic AI, platforms like CareNexus unify care delivery and claims economics, automate workflows, and deliver measurable improvements in outcomes and cost. Built on Microsoft Power Platform and Azure, CareNexus combines clinical context, operational intelligence, and financial insight—closing the loop between care and claims.
The Industry Challenge: Why Claims Alone Can’t Solve Rising Costs
Claims systems were designed for financial adjudication, not care delivery. They excel at processing transactions but fail to address the complexity of healthcare journeys. This gap has real consequences: fragmented care pathways lead to delays, unnecessary interventions, and escalating costs.
Consider musculoskeletal (MSK) injuries—a leading driver of workers’ compensation claims. According to the Canadian Institute for Health Information (CIHI), MSK injuries account for up to 40% of claims and billions in annual costs. Delays in triage and inconsistent pathway adherence can extend claim duration by 20–30%, increasing both direct and indirect costs. Traditional claims platforms cannot prevent these inefficiencies because they lack visibility into clinical workflows and provider performance.
Claims systems adjudicate the past. Coordinated Care Intelligence orchestrates the future.
The Market Signal: Coordinated Care Is Becoming Strategic
The shift toward care orchestration is no longer theoretical—it’s happening now. WSIB’s Executive VP recently stated:
“We have identified the missing piece of the puzzle. We’re training care coordinators to manage worker care journeys.”
This reflects a growing recognition that financial adjudication alone cannot deliver sustainable results. Similar initiatives are emerging in auto insurance and workers’ compensation programs across North America, driven by regulatory pressures and outcome-based reimbursement models.
Manual coordination, however, is a stopgap solution. It requires significant staffing, introduces variability, and cannot scale across diverse programs. The future demands digital intelligence—platforms that automate coordination, enforce evidence-based pathways, and provide real-time visibility into outcomes and costs.
Defining Coordinated Care Intelligence
Coordinated Care Intelligence represents a new category of technology designed to close the gap between care delivery and claims management. Unlike claims platforms, which focus on financial transactions, these systems integrate clinical context, operational workflows, and economic metrics into a single, actionable framework.
At its core, Coordinated Care Intelligence enables payers to move from reactive adjudication to proactive orchestration. It ensures that every care decision—whether triage, provider assignment, or discharge planning—is informed by policy, evidence, and cost implications. This approach not only improves patient outcomes but also reduces unnecessary interventions and accelerates recovery timelines.
Coordinated Care Intelligence is the bridge between better care and better economics.
The Role of Agentic AI
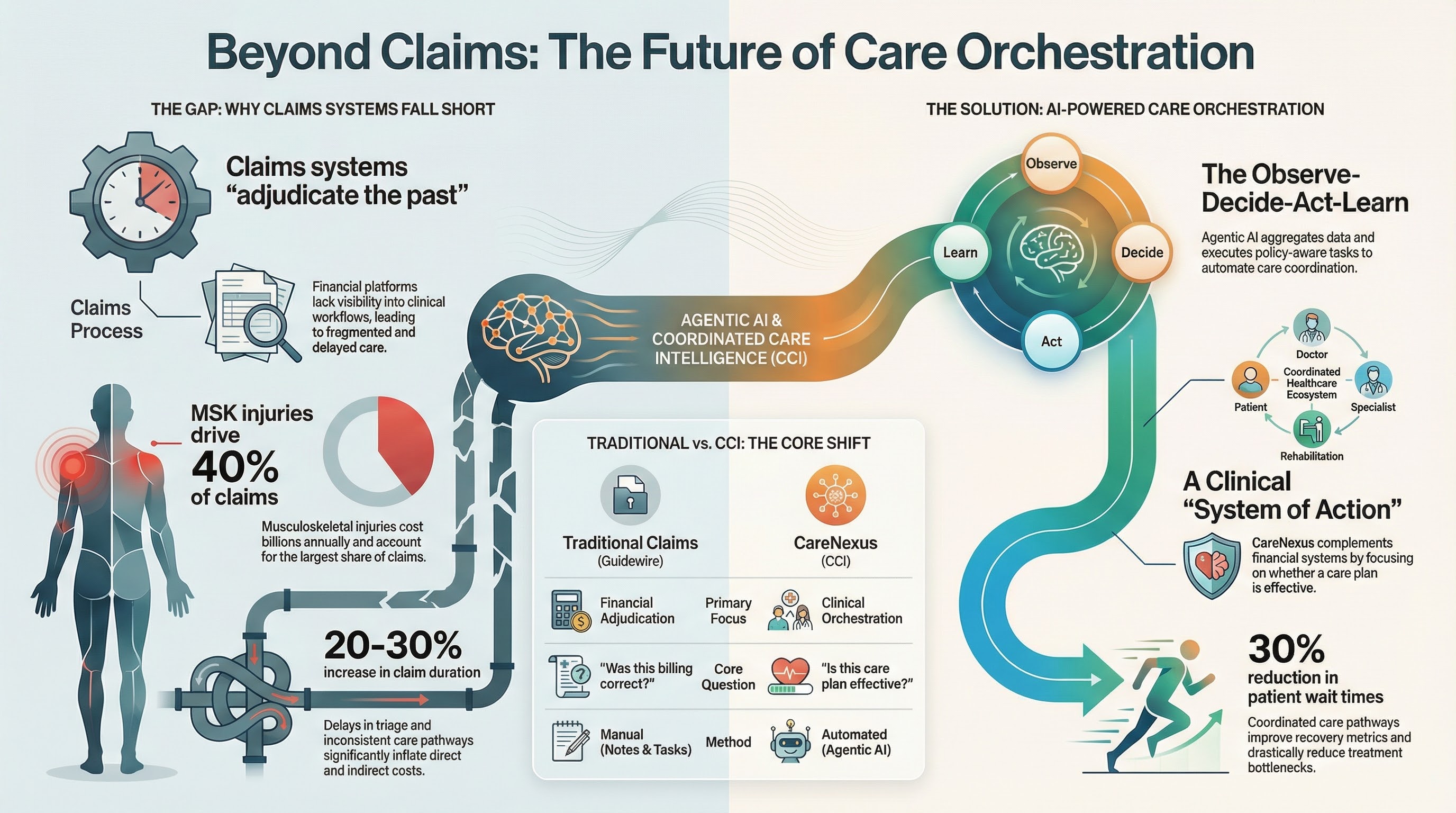
Agentic AI represents a fundamental shift in governed care coordination. Unlike advisory models, it is designed to act—but only within a strict, auditable framework. Built on Microsoft’s Responsible AI principles and to be PHIPA/PIPEDA compliant, every action is policy-aware and subject to human-in-the-loop oversight.
This governance-first approach allows Agentic AI to safely augment human judgment, not replace it, by autonomously performing the high-volume, low-complexity tasks that slow down care. It doesn't replace human judgment; it augments it, ensuring that manual coordination—which is slow, costly, and prone to variability—is made efficient and consistent.
The Observe → Decide → Act → Learn cycle is the backbone of this intelligence:
- Observe: Aggregate referrals, assessments, and historical outcomes into a unified context using Dataverse.
- Decide: Apply evidence-based triage rules and payer policies to recommend next steps.
- Act: Execute administrative tasks—drafting letters, creating tasks, routing workflows—inside CareNexus modules.
- Learn: Feed outcomes back into CareInsights dashboards, enabling continuous improvement of pathways and cost models.
This is not theoretical. In WSIB’s environment, where Guidewire handles claims adjudication, Agentic AI can bridge the gap by orchestrating care journeys in real time—something claims systems were never designed to do.
Business Impact: Closing the Loop Between Care and Claims
The economic case for Coordinated Care Intelligence is compelling. Claims platforms focus on financial accuracy, but they cannot influence the upstream drivers of cost: delayed care, unnecessary interventions, and fragmented provider networks. These inefficiencies inflate indemnity costs and prolong wage-loss exposure.
By embedding Agentic AI into care coordination, payers can:
- Protect Loss Ratios: Reduce over-medicalization by enforcing evidence-based pathways, cutting unnecessary diagnostics and directly lowering claim costs.
- Accelerate Recovery & RTW: Coordinated care shortens time-to-treatment, improving return-to-work (RTW) metrics—a critical KPI for WSIB and all work-injury payers. This directly reduces wage-loss exposure and indemnity costs.
- Lower Administrative Expense: AI-driven documentation and workflow automation free staff for high-value case management, reducing operational overhead and improving team productivity.
ROI Modeling:
For a payer managing 50,000 MSK claims annually, our data on pathway optimization shows CareNexus can reduce the average claim duration. Even a 10% reduction in duration for this cohort, based on an average daily wage-loss cost, can translate into millions in direct savings. WSIB’s own data shows that prolonged MSK claims significantly impact loss ratios. By integrating CareNexus, these claims are managed proactively—linking every care decision to its economic impact.
Closing the Gap: How CareNexus Complements Claims Platforms
Coordinated Care Intelligence (CCI) does not replace core claims systems; it enhances them. Claims platforms are the financial system of record, while CareNexus is the clinical system of action.
Case Example: WSIB Ontario and Ontario Workers Network (OWN)
WSIB Ontario operates one of the largest workers’ compensation programs in Canada, processing thousands of claims through Guidewire. While Guidewire ensures financial adjudication, it does not manage the complexity of care delivery. Recognizing this gap, WSIB has invested in training care coordinators—a clear signal that proactive care orchestration is now strategic.
The Ontario Workers Network (OWN) provides a blueprint for what coordinated care can achieve. OWN connects providers across the province to deliver evidence-based MSK care. CareNexus powers this network, automating triage, provider assignment, and documentation while feeding real-time insights into dashboards for program managers.
Impact Highlights:
- Coordinated care pathways reduced wait times by up to 30%.
- AI-driven triage improved adherence to evidence-based guidelines by over 45%, reducing costly pathway deviations.
- Real-time dashboards provided managers with 100% visibility into provider performance, identifying and resolving care bottlenecks 3x faster than manual audits.
This is the future moving toward: a hybrid model where claims adjudication (Guidewire) and care orchestration (CareNexus) work in tandem—supported by Agentic AI.
Call to Action
The industry is at an inflection point. Early adopters of Coordinated Care Intelligence will gain a competitive advantage—reducing costs, improving outcomes, and meeting regulatory demands.
Book a demo to see CareNexus in action and explore how Agentic AI can transform your care coordination strategy





